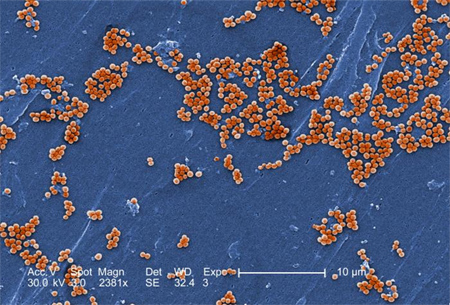
CTV news reports that methicillin-resistant Staphylococcus aureus killed 2300 Canadians in 2006. The Public Health Agency of Canada gathered the data through a national surveillance program undertaken in 48 Canadian hospitals. The data collection samples a cross section of institutions chosen to represent all Canadian hospitals.
An estimated 2,300 Canadians died in 2006 after contracting antibiotic resistant Staph bacteria, costing the national heath-care system between $200 million and $250 million that year, new figures suggest.
The figures, based on data gathered from a, indicate doctors saw 29,000 new patients carrying methicillin-resistant Staphylococcus aureus (MRSA) bacteria on their skin or nostrils in 2006.Of those, 11,700 contracted new MRSA infections.
MRSA, one of the strongest drug-resistant bacteria currently known, can live on human skin without causing infection. However, if it gains entry to the body through a cut or wound, it can cause serious illness and death, according to the Mayo Clinic’s website.
MRSA infections are often contracted by patients who are already in the hospitals…
Dr. Andrew Simor, the chief of microbiology and infectious diseases at Toronto’s Sunnybrook Health Sciences Centre, co-chairs the surveillance program. He said the 2006 figures show a slow but steady increase over previous years.
“The good news is our rates remain substantially less than what is seen in the United States and many other parts of the world,” Simor told The Canadian Press.
According to the report, 62 per cent of the new MRSA cases reported in 2006 were acquired in hospitals.
Dr. Michael Gardam, the director of the University Health Network’s Infection Prevention and Control Unit in Toronto, says he’s glad to see this dangerous infection finally getting some attention.
“MRSA has been around for 40-50 years,” he told CTV’s Canada AM on Thursday. “This isn’t new. It’s amazing that only in the last few years is the public starting to hear about this.
“This is the untold secret of hospitals. People can come in for some reason and then end up dying from something they caught in the hospital.”
He said that thanks to the SARS epidemic of 2003, hospitals are slowly but surely improving their techniques for preventing such infectious diseases.
Health professionals also say medical personnel need to be vigilant about hygiene.
“In a hospital setting, infection control is paramount,” said Dr. Donald Low, the senior microbiologist at Toronto’s Mount Sinai Hospital.
“We have to enforce proper infection control procedures: hand washing, these things are now being taken seriously in the last couple of years, whereas before we paid more lip service to it.”
MRSA reaching beyond hospitals
Community-acquired MRSA accounted for 15 per cent of the cases reported in the study. The rest were acquired in long-term care facilities, hospitals outside the monitored network or were of unknown origin.
The rate of MRSA cases acquired outside hospitals has nearly doubled over the past five years, according to Simor.
The strain of bacteria more common in community settings usually causes persistent skin infections, but can also trigger severe pneumonia and bloodstream infections.
The community-acquired cases addressed in the report are not representative of the actual number of infections, as they only include the cases that were bad enough to prompt the infected to seek hospital care — not those treated by a family doctor or in a clinic.
The increase in such cases is viewed by disease control experts as an alarming trend, particularly as they more often involve people who don’t fit the profile for MRSA infection.
This movement is something that concerns Dr. John Conly. Head of the department of medicine at University of Calgary, he has been following community acquired MRSA in the city and says what used to be common only in marginalized groups is spreading to the general population.
“We’re seeing now probably 20 per cent to 30 per cent (of infection cases) where we have no logical explanation,” he said, noting community acquired cases are actually outpacing those stemming from hospitals in a few areas.
According to the director general of the Public Health Agency’s centre for communicable diseases and infection control, more needs to be done to fight MRSA in hospitals and in the community.
Dr. Howard Njoo said containing the resilient bacteria is one of the most important battles to win from the perspectives of both disease prevention and cost effectiveness.
With files from The Canadian Press
The best protection against bacterial infection is frequent hand-washing with soap.